- (503) 575-0134
- hello@awakeningscounselingpnw.com
- Online Therapy in Seattle, WA and Across Washington

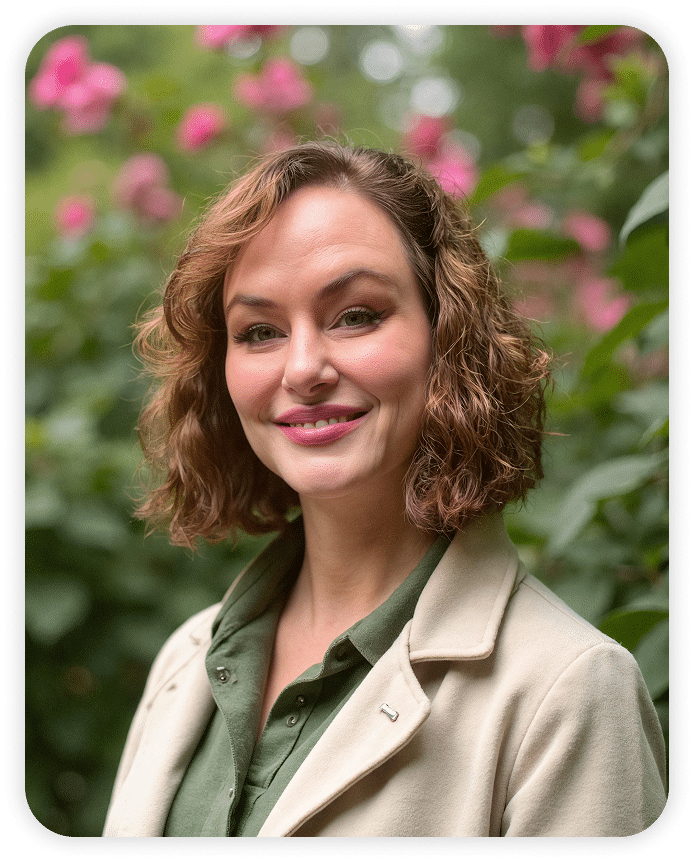
As a trauma therapist in Washington State serving Seattle, Tacoma, Bellevue, Spokane & online. I guide people to heal from complex PTSD rooted in long-term trauma. Through methods like EMDR, IFS (parts work), somatic therapy, and Ketamine-Assisted Psychotherapy (KAP), we’ll safely explore what’s beneath the surface.
You were not born this way. We all enter this world as a blank slate. Then, life happens. Experiences and events. Traumas and triumphs. Parents and partners.
Trauma therapy can help you explore:
These pathways are not personal flaws – they’re survival patterns your brain learned to protect you from chronic chaos and crisis. But protection isn’t the same as peace, and now, you get to choose something new.
When you choose to heal, it changes the way your mind works, and you don’t just feel better – you live differently.
Some days, you feel frozen—numb, detached, exhausted. Other days, your emotions feel too big to hold. You might not always call it trauma. But the way you carry it—in your body, your relationships, and your inner dialogue—tells its own story.
Complex trauma (C-PTSD) often stems from prolonged, repeated trauma, especially in childhood relationships where adequate safety and care were missing. You’ve learned to stay small, stay alert, or stay busy to protect yourself—but it’s left you emotionally overwhelmed, disconnected, and trapped in survival mode.
The symptoms of complex trauma can show up in insidious ways. You might notice:

If you’re ready to take the next step, please book a consultation or request an appointment today!
Go From This:
To This:
Trauma therapy helps you feel safe in your own body, reconnect with your emotions, and shift the patterns that once protected you but now keep you stuck. You begin to trust yourself, speak your needs, and soften the constant inner tension.
Healing from complex PTSD doesn’t mean forgetting what happened. It means learning to live in your body again—without fear, shame, or hypervigilance.
Life after trauma can feel more spacious. You sleep better. You stop apologizing for yourself. You show up in relationships with clarity, rather than fear. It doesn’t happen overnight—but with the right support, healing becomes your new reality. This trauma treatment in Seattle, WA, helps you reclaim your life.


Our sessions are a space where your body can finally exhale. Where you’re no longer surviving—you’re rising.
The healing process isn’t linear, it’s circular. Messy. Imperfect. Disruptive. And worth every step. Together, we’ll co-explore your story, so you can:
Licensed trauma therapist serving Seattle, Tacoma, and greater Washington State.
In our work together, we’ll move at your pace. This is not about forcing change—it’s about building safety and connection, so sustainable healing can happen.
I offer trauma-informed approaches that may include:
All that truly matters is what you do right now - Invest In Yourself.

The part of you that reaches for alcohol, weed, or pills isn’t reckless—it’s protective. In IFS therapy, we call this a firefighter protector part. It shows up fast when pain overwhelms—intrusive memories from the past, strained relationships, the pressure to hold everything together—and it tries to make it STOP.
This part has helped you survive what your nervous system never got to process. It’s soothed the guilt, the fear, the ache of always feeling “too much” or “never enough.” In therapy, we don’t fight or shame this part. We listen. And we show it there’s another way to feel safe. Working with a trauma therapist in Washington State provides compassionate addiction support.
When love has felt unsafe in the past, it’s natural to feel anxious, avoidant, and fearful in relationships now. You might cling too tightly or pull away the moment things get real. These aren’t personal flaws—they’re protective responses your nervous system learned to survive relational trauma.
It makes sense if emotional intimacy feels like a push-pull dance. You long for connection but brace for rejection and abandonment. Therapy can help you gently explore where those patterns come from—so you can begin building relationships that feel steady, mutual, and safe to stay in.

You learned early that your needs had to come last. That love meant overextending, overfunctioning, and absorbing other people’s pain and chaos. For years, codependency felt like connection. But deep down, a quiet voice kept asking—what about me? And maybe estrangement became the last resort—and the first time you listened to yourself.
Even if walking away brought relief, it may have also brought grief, guilt, and second-guessing. But choosing yourself after years of self-betrayal isn’t selfish—it’s sacred. In therapy, we’ll untangle those patterns and help you rebuild from a place of self-love, not self-abandonment.
Complex trauma often creates an irreconcilable, invisible war inside. You might feel disconnected from your body, unsure of what you want, and flooded with shame for even having needs. Criticism cuts deep. Boundaries feel impossible. And receiving love and care? That can feel more threatening than comforting.
Therapy can be a space to reclaim what trauma tried to take—your voice, your worth, your trust in yourself. Together, we’ll explore the protective patterns like crippling self-doubt, people-pleasing, or abandoning your needs, and begin to build a relationship with yourself that’s rooted in authenticity and self-love, not fear.
Get started with a trauma-informed therapist in the state of Washington.
Complex PTSD
Complex PTSD is When Survival Mode Becomes Your Baseline
C-PTSD presents in ways that are hard to explain—emotional flashbacks, sudden shutdowns, or a deep-seated fear of being inherently flawed. You might feel haunted by your past, even if you can’t pinpoint exactly why. You just know you’re exhausted from carrying it alone.
Many people with complex trauma struggle to feel at ease in their own bodies, relationships, or daily lives. If you’ve spent years in survival mode, trauma-informed therapy can help you understand why—and begin the slow, supportive work of reconnecting with safety, trust, and yourself.
Anxiety
Anxiety is When Your Mind Never Stops Moving
Anxiety can feel like your brain is hijacked in overdrive—planning, analyzing, worrying, fixating, preparing for the worst. Even when things are calm, your body and mind stay braced. You might feel restless, on edge, or flooded with unwanted thoughts that never seem to stop and let you rest.
Maybe it shows up as catastrophizing, over-performing, or the inability to relax. You’re not paranoid or broken—you’re exhausted from operating in hypervigilance mode for too long. Therapy can help you slow down, loosen the grip of tension in your body, and finally catch your breath.
Depression
Depression is When You’re Tired of Pretending You’re Fine
Depression can feel like dragging yourself through each day with a weight no one else sees. You might feel disconnected from pleasure, zapped of life energy, or overwhelmed by even the smallest tasks—like making dinner, replying to a text, or getting out of bed.
You may notice changes in sleep, appetite, concentration, or libido. Maybe you’re isolating more, falling back into old coping habits, or wondering why everything feels so hopeless. Therapy offers a space to gently explore what’s underneath the heaviness—and begin finding your way back to yourself.
Substance Abuse
Substance Abuse is When Numbing Became the Only Way to Get Through
Substance abuse doesn’t always start with recklessness—it often starts with pain. Maybe it was a way to quiet your thoughts, escape the past, or simply make life feel bearable. Over time, what felt like relief may have become a cycle that’s now impossible to break.
You might feel torn between guilt and craving, between wanting change and fearing what will happen if you do. This isn’t about willpower—it’s about adaptation and survival. Therapy can help you understand the parts of you that turned to substances and begin building safer ways to cope, connect, and heal.
Behavioral Addictions
Behavioral addictions—like gambling, compulsive eating, shopping, scrolling, or overworking—can quietly take hold when you’re just trying to get through the day. They offer quick relief, but often leave you feeling numb, ashamed, or out of control once the moment passes.
These patterns don’t mean you’re defective—they’re signals of deeper pain your nervous system has worked hard to manage. Therapy can help you understand the role these behaviors play, reduce shame, and begin finding more sustainable ways to self-soothe and regulate your emotions.
Complex trauma often shows up in ways that don’t neatly fit into any one diagnosis—but that doesn’t make your pain any less real. At Awakenings Counseling, rather than focus on “ballpark” diagnoses, I offer holistic trauma-informed therapy that helps you make sense of your past, reclaim your life, and move toward healing with compassion and clarity. Trauma treatment in Washington State can be a space to reclaim what trauma tried to take.
EMDR
EMDR for Complex Trauma, PTSD, Addiction, Anxiety and Depression
EMDR (Eye Movement Desensitization and Reprocessing) is a form of psychotherapy used to treat trauma and other distressing experiences. It involves focusing on traumatic memories while engaging in bilateral stimulation, typically eye movements, to help process and reduce the symptoms associated with trauma—anxiety, fear, terror, flashbacks, sleep problems and addiction.
By definition, trauma is an experience that is so overwhelming in the moment that it cannot be processed and is locked away in its own neural network.
EMDR helps the rest of the brain, with its innate healing resources, connect with the traumatic memory network to process, integrate, and resolve the troubling memory.
Like dreaming, which involves bi-lateral eye movements, EMDR activates a similar type of brain processing that enables us to put the traumatic memories behind us, only keeping what knowledge, wisdom, and self-empowerment we need.
Ketamine-Assisted Psychotherapy (KAP)
Ketamine-Assisted Psychotherapy (KAP) for Complex Trauma, PTSD, Addiction and Depression
Ketamine-Assisted Psychotherapy (KAP) is a holistic modality in which ketamine is used as a complement to psychotherapy to help eligible clients experience more frequent breakthroughs and sustained improvement in symptoms. When traditional treatments like talk therapy and medications provide limited relief, KAP can be a more effective solution.
Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy (ACT) for Anxiety, Depression and Substance Abuse
In essence, ACT aims to improve psychological flexibility, which involves:
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) for Complex Trauma, PTSD, Anxiety and Depression
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) is an evidence-based treatment designed to help individuals process and cope with traumatic experiences.
TF-CBT aims to help individuals manage PTSD symptoms, improve emotional regulation, and develop healthy coping mechanisms, which involves:
Psychoeducation
TF-CBT provides education about trauma, its effects on the individual, and the normal reactions to traumatic events.
Trauma Narrative
This involves helping the individual create a narrative of their traumatic experience, allowing them to explore and process the events in a safe and controlled manner.
Cognitive Processing
TF-CBT helps individuals identify and challenge unhelpful or distorted thoughts and beliefs related to the trauma.
Relaxation Techniques
TF-CBT incorporates relaxation techniques like deep breathing or mindfulness to help manage anxiety and reduce physiological symptoms of distress.
Coping Skills
Individuals learn various coping mechanisms, such as assertiveness training and problem-solving skills, to manage daily stressors and prevent retraumatization.
Internal Family Systems (IFS)
Internal Family Systems (IFS) Therapy for Complex Trauma, PTSD, Addiction, Anxiety and Depression
Internal Family Systems (IFS) Therapy offers a compassionate, holistic approach to healing trauma by acknowledging and integrating different aspects of the personality, often referred to as “parts,” to promote healing and wholeness.
IFS therapy distinguishes between the “Self” (the core of compassion and wisdom) and various protector “parts” that hold beliefs, emotions, and behaviors shaped by experiences, including trauma.
By fostering internal dialogue and understanding between these parts, IFS therapy aims to release burdens, integrate wounded parts, and restore balance within the individual’s internal system.
Somatic Therapy
Somatic Experiencing Therapy for Complex Trauma, PTSD, Anxiety and Depression
Somatic Experiencing is a body-oriented approach that helps individuals release physical and emotional tension stored in the body due to past traumatic experiences.
It focuses on the body’s natural healing abilities by guiding individuals to become more aware of their bodily sensations and to process and release trauma through gentle, mindful movements and exercises.
Mind-Body Connection
Somatic Experiencing emphasizes the strong connection between the mind and body, recognizing that trauma can manifest in physical symptoms like chronic tension, pain, and emotional dysregulation.
Somatic Awareness
This therapy involves learning to pay attention to physical sensations, including those associated with trauma, and to notice how the body responds to different emotions and experiences.
Gradual Release
Instead of directly confronting traumatic memories, Somatic Experiencing gently encourages individuals to process and release stored tension and trauma through a gradual process of becoming more aware of their body and its reactions.
Self-Regulation
The goal is to help individuals regain control over their nervous system and develop self-regulation skills, enabling them to respond to life’s challenges with greater flexibility and resilience.
Motivational Interviewing (MI)
Motivational Interviewing (MI) for Addiction, Anxiety and Depression
Motivational Interviewing (MI) is a client-centered, goal-oriented approach designed to help individuals resolve ambivalence about change and increase their motivation to make positive behavioral changes.
It focuses on exploring and strengthening a person’s own reasons for change, rather than directly advising or persuading them.
Empathy and Reflective Listening
Therapists use reflective listening to show understanding and respect, fostering a collaborative relationship where clients feel heard and supported.
Exploration of Ambivalence
MI recognizes that ambivalence (having conflicting feelings about change) is a natural part of the process and helps individuals navigate these feelings.
Developing Discrepancy
Therapists help clients see the gap between their current behavior and their desired goals, highlighting the reasons for change.
Supporting Self-Efficacy
MI emphasizes the client’s ability to change, fostering belief in their capacity to make positive changes.
Rolling with Resistance
Instead of confronting resistance, therapists help clients explore their reasons for not wanting to change, validating their feelings and promoting exploration.
Change Talk
MI focuses on eliciting and reinforcing “change talk,” which are statements expressing a desire to change, a problem with current behavior, an ability to change, and a reason or need to change.
Prolonged or Repetitive Trauma
C-PTSD is most often associated with experiences like childhood abuse (physical, verbal, emotional, or sexual), ongoing domestic violence and relational discord, and the inability to leave, where the traumatic events are repeated or last for a considerable duration.
Childhood Trauma
Early life trauma, particularly during formative years, can have a profound and lasting impact on development. In addition to abuse, neglect is also a factor when caregivers fail to adequately meet a child’s basic needs, including physical, emotional, medical and educational.
Witnessing Violence
Exposure to domestic violence, substance abuse, community and socioeconomic violence, suicide, or criminal activity that includes physical assault, sexual assault, assault with a deadly weapon, and homicide.
Lack of Escape or Control
Traumatic experiences and environments that are difficult or impossible to escape from, or where individuals feel powerless to control their circumstances or outcomes.
Harm by Someone Close
Trauma inflicted by someone who is supposed to be a caregiver or protector can be particularly damaging, especially when mental illness and addiction are present.
The Adverse Childhood Experiences (ACE) Questionnaire for Adults summarizes 10 categories of traumatic experiences from birth to age 18.
This questionnaire can be found online for free, and it is a powerful tool for identifying your trauma score (0-10).
Perhaps you didn’t experience severe abuse and neglect, or you grew up with socioeconomic stability where your needs were met.
From the outside looking in, your family appeared normal. That’s where relational trauma comes into play, when the people who were supposed to love you caused the most harm.
Complex trauma often begins with parenting that lacked the stability, safety, and unconditional love every child deserves. This is especially true in cases of attachment trauma—where emotional neglect, inconsistent caregiving, or chronic invalidation left you feeling unseen, unheard, or like your needs were a burden. Over time, this kind of early relational harm lays the foundation for CPTSD, shaping how you view yourself and others in adulthood.
Emotional abuse, particularly narcissistic abuse, may never leave a bruise—but it wounds even deeper. You may have been gaslit, given the silent treatment, or made to feel worthless. Love may have been used as a reward, withheld when you didn’t comply. The constant criticism, manipulation, and fear-based control can leave you with lingering shame and a belief that you’re fundamentally flawed. You’re not. These are the effects of trauma—not reflections of your inherent worth.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a handbook published by the American Psychiatric Association (APA) that provides standardized diagnostic criteria for mental health disorders. The DSM is used by healthcare professionals to diagnose and treat mental health disorders.
Post-traumatic stress disorder (PTSD) is a mental health disorder that can occur after experiencing or witnessing a traumatic event. The DSM-5, the most recent edition of the DSM, includes PTSD as a diagnosis.
The DSM-5 does not include Complex PTSD (C-PTSD) as a separate diagnosis, but instead considers it a subtype of PTSD. This decision was based on research that found that 92% of individuals with C-PTSD also met the diagnostic criteria for PTSD.
While the DSM-5 does not include C-PTSD as a separate diagnosis, it does acknowledge the existence of complex trauma and the potential for unique symptoms and experiences that may not be captured by the PTSD diagnosis alone.
Complex PTSD (C-PTSD) is often associated with other comorbid mental health disorders due to overlapping symptoms and a lack of widespread awareness about the nature of C-PTSD. Some examples include:
C-PTSD is a common thread in comorbid disorders that is rooted in chronic exposure to traumatic experiences.
It depends on the level of acuity of the substance abuse/addiction. For chronic and/or severe substance use, it is imperative to seek inpatient rehabilitation or intensive outpatient substance use disorder counseling.
Psychotherapy is an adjunctive treatment for dual diagnosis, and is most effective when coupled with sobriety and a commitment to recovery.
Absolutely.
Seeking therapy is highly recommended when a loved one is struggling with mental illness or addiction, as it can provide valuable support and coping strategies for both the individual and the family.
Therapy helps family members understand the illness and learn how to effectively support their loved one’s recovery.
How therapy is beneficial in this situation:
Ketamine is a medicine used to treat a variety of mental health conditions, including depression, anxiety and PTSD. Ketamine has rapidly-acting antidepressant and mood-enhancing effects, which can begin to take effect within 1-2 hours after treatment and last for up to 2 weeks. It works by blocking the brain’s NMDA receptors as well as by stimulating AMPA receptors, which are thought to help form new synaptic connections and boost neural circuits that regulate stress and mood. Ketamine has also been shown to enhance overall neuroplasticity—the brain’s natural capacity to change and adapt—for lasting symptom improvement.
How Does Ketamine Feel?
The effects of ketamine, which most clients find pleasant, last for approximately 45 minutes. These effects can make you feel “far from” your body, and facilitate shifts in perception that can often feel expansive in nature. Your motor and verbal abilities will be reduced, so you’ll be lying down in a comfortable position during the experience. You can listen to ambient music and wear an eye mask to be as relaxed as possible.
What Are Integration Sessions?
Within 24 to 48 hours following a ketamine session, often referred to as a “critical period,” during which enhanced brain plasticity peaks, we’ll spend your follow-up therapy session giving you space to process the memories, thoughts & insights that arose during your dosing session.
How Does Ketamine-Assisted Psychotherapy Work?
Schedule an initial consultation with a psychiatric medical practitioner at a KAP provider of your choice for either at-home or in-clinic treatments.
They will review your medical and psychiatric history with you, provide education on the treatment and determine if you are eligible for KAP.